What is the Cornea?
Cornea Transplant Surgery, DMEK Surgery and Fuchs Dystrophy
The newest and most effective treatment for Fuchs dystrophy and other causes of corneal endothelial cell dysfunction is a surgery called “DMEK.”
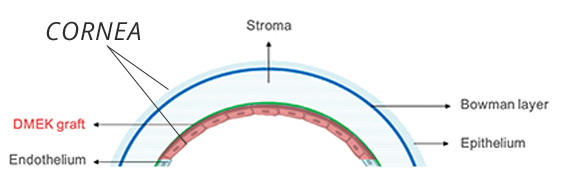
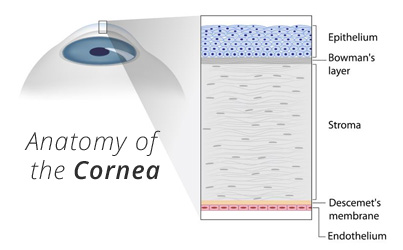
DMEK stands for Descemet’s membrane endothelial keratoplasty, a procedure that involves transplanting only a single layer of cells of the inner cornea (the corneal endothelium) – only about 2% of the total corneal thickness. DMEK is the newest and most technically difficult form of corneal transplantation to perform, but it can result in better visual outcomes, lower rates of graft rejection, and faster healing than other techniques. Due to the difficulty in mastering this new technique, DMEK is not as commonly performed as simpler operations. However, the excellent results with DMEK have led more surgeons around the United States to begin performing the surgery in patients with Fuchs dystrophy and those with disease limited to the corneal endothelium (inner layer).

Dr. Geoffrey Hill is among the very first cornea specialists performing DMEK surgery in the greater St. Louis area.
At Hill Vision Services, we provide a full range of corneal transplantation techniques for patients with corneal disease. In patients who are not candidates for DMEK surgery, other techniques for partial-thickness and full-thickness corneal transplants can be performed (see below).
Click here to learn more about Fuchs dystrophy at the Fuchs Friends patient forum.
Cornea transplant surgery is also for patients with:
Keratoconus
Corneal scarring from infection or injury
Rare corneal dystrophies affecting corneal clarity
What is a corneal transplant, and how is it performed?
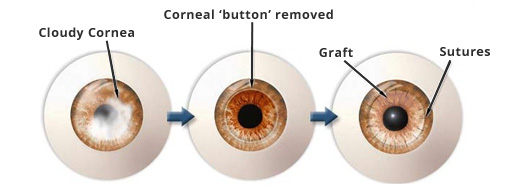
Over the past 50 years, ophthalmologists have developed techniques to replace cloudy corneas and restore vision by performing corneal transplant surgeries. This type of surgery replaces the damaged cornea with clear corneal tissue from a human organ donor.
Full-thickness corneal transplants (for corneal clouding or scarring) are performed by removing a full-thickness, central, circular piece of the damaged cornea and sewing a replacement piece of donor tissue in its place. These kinds of grafts are called “penetrating keratoplasties” (or PKPs) because they involve replacing the entire thickness of the damaged cornea. To continue the wristwatch analogy, this would be like replacing the damaged or cracked crystal covering of your wristwatch with a clear new piece of crystal.
Is having a corneal transplant similar to having a liver or kidney transplant?
In some ways, yes. It is similar, although having a corneal transplant does not require taking the same lifelong regimen of medications as after a solid organ transplant. The transplanted corneal tissue comes from a human donor who has undergone very strict testing to make sure they are disease-free. Keeping the graft healthy requires taking some medications – usually only eye drops – to help decrease inflammation and to prevent the immune system from rejecting the transplanted tissue.
Cornea donation and the process of eye banking have a fascinating history and have allowed ophthalmologists to restore sight for millions of patients around the world. For readers who are interested in learning more, visit the Missouri Lions Club website.
